Type 2 diabetes is a chronic condition that affects the way the body processes blood sugar (glucose). Unlike Type 1 diabetes, which is characterized by the body’s inability to produce insulin, Type 2 diabetes occurs when the body becomes resistant to insulin or when the pancreas does not produce enough insulin. This form of diabetes is more common and typically develops in adults, although increasing numbers of children are being diagnosed. This comprehensive guide explores the symptoms, causes, treatment options, and management strategies for Type 2 diabetes.
Symptoms of Type 2 Diabetes
Identifying the symptoms of Type 2 diabetes early can lead to more effective management and prevention of complications. Common symptoms include:

- Increased Thirst and Frequent Urination: High blood sugar levels lead to excessive thirst (polydipsia) and frequent urination (polyuria).
- Increased Hunger: The body’s inability to use glucose effectively causes increased hunger (polyphagia).
- Unintended Weight Loss: Despite eating more, people with Type 2 diabetes might lose weight as the body uses fat and muscle for energy.
- Fatigue: Insufficient glucose in cells leads to feelings of fatigue and tiredness.
- Blurred Vision: High blood sugar can cause swelling in the lenses of the eyes, resulting in blurred vision.
- Slow-Healing Sores or Frequent Infections: Poor blood circulation and high glucose levels impair the body’s ability to heal.
- Darkened Skin: Areas of dark, velvety skin (acanthosis nigricans), particularly in the neck and armpits, can be a sign of insulin resistance.
Also Read:- The 5 Essential Components of Diabetes Management Strategy
Causes and Risk Factors
Type 2 diabetes is primarily influenced by lifestyle factors and genetics. Key causes and risk factors include:

- Genetic Factors: A family history of Type 2 diabetes increases the risk.
- Obesity and Physical Inactivity: Excess body fat, particularly around the abdomen, and a sedentary lifestyle are significant risk factors.
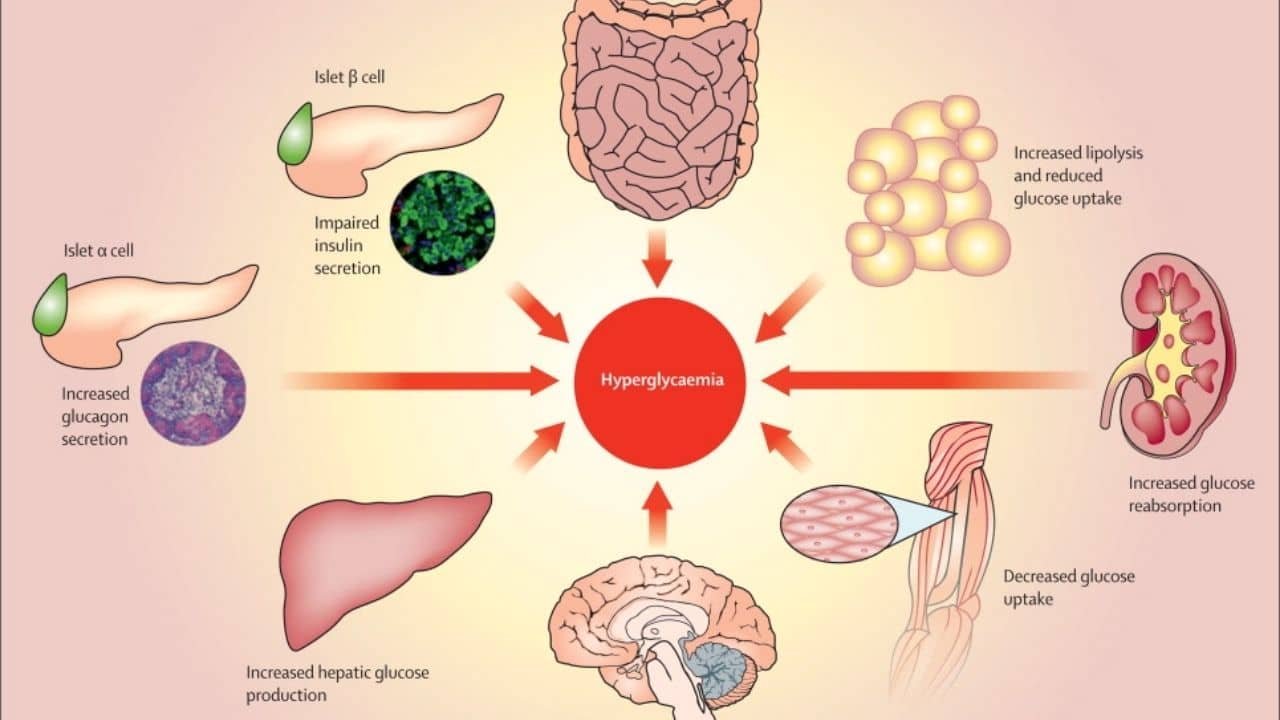
- Insulin Resistance: Cells in the muscles, liver, and fat become resistant to insulin, necessitating higher insulin production.
- Age: The risk of Type 2 diabetes increases with age, especially after 45 years.
- Ethnicity: Certain ethnic groups, including African Americans, Hispanics, Native Americans, and Asian Americans, are at higher risk.
- Polycystic Ovary Syndrome (PCOS): Women with PCOS have a higher risk of developing Type 2 diabetes.
- High Blood Pressure and Abnormal Cholesterol Levels: These conditions are often associated with Type 2 diabetes.
Diagnosis
Diagnosing Type 2 diabetes involves several tests, including:

- Glycated Hemoglobin (A1C) Test: This test measures average blood sugar levels over the past 2-3 months. An A1C level of 6.5% or higher indicates diabetes.
- Fasting Blood Sugar Test: Blood sugar levels are measured after an overnight fast. A level of 126 mg/dL or higher indicates diabetes.
- Oral Glucose Tolerance Test (OGTT): Blood sugar levels are measured before and two hours after consuming a sugary drink. A two-hour blood sugar level of 200 mg/dL or higher indicates diabetes.
- Random Blood Sugar Test: A blood sample is taken at a random time. A level of 200 mg/dL or higher suggests diabetes.
Treatment and Management
While there is no cure for Type 2 diabetes, it can be managed effectively through a combination of lifestyle changes, medications, and regular monitoring.
Lifestyle Changes
Adopting a healthy lifestyle is crucial for managing Type 2 diabetes:
Balanced Diet: Focus on a diet rich in vegetables, fruits, whole grains, lean proteins, and healthy fats. Limit intake of refined sugars and carbohydrates.
Regular Physical Activity: Aim for at least 150 minutes of moderate aerobic exercise or 75 minutes of vigorous exercise per week, along with muscle-strengthening activities.
Weight Management: Losing even a small amount of weight can improve blood sugar control and overall health.
Medications
Several types of medications can help manage Type 2 diabetes:

- Metformin: Often the first medication prescribed, it reduces glucose production in the liver and improves insulin sensitivity.
- Sulfonylureas: These drugs help the pancreas produce more insulin.
- Meglitinides: Stimulate quick insulin production in response to meals.
- Thiazolidinediones: Improve insulin sensitivity.
- DPP-4 Inhibitors: Help reduce blood sugar levels without causing low blood sugar.
- GLP-1 Receptor Agonists: Slow digestion and help lower blood sugar levels.
- SGLT2 Inhibitors: Help the kidneys remove glucose from the bloodstream.
Blood Sugar Monitoring
Regular blood sugar monitoring is essential for managing Type 2 diabetes:
Self-Monitoring: Use a glucometer to check blood sugar levels regularly.
Continuous Glucose Monitoring (CGM): Provides real-time blood sugar readings and trends.

Education and Support
Education and support are key components of diabetes management:
Diabetes Education Programs: These programs offer guidance on managing diabetes, including diet, exercise, and medication adherence.
Support Groups: Joining a diabetes support group can provide emotional support and practical advice.
Complications and Prevention
If not properly managed, Type 2 diabetes can lead to serious complications:
- Cardiovascular Disease: Increased risk of heart attack, stroke, and atherosclerosis.
- Neuropathy: Nerve damage, especially in the legs, leading to pain and numbness.
- Nephropathy: Kidney damage, potentially resulting in kidney failure.
- Retinopathy: Eye damage, increasing the risk of blindness.
- Foot Damage: Poor circulation and nerve damage can lead to serious foot infections and, in severe cases, amputation.
Preventing complications involves:
Regular Medical Check-ups: Routine visits to healthcare providers to monitor blood sugar levels and overall health.
- Healthy Lifestyle Choices: Maintaining a balanced diet, regular exercise, and avoiding smoking and excessive alcohol consumption.
- Medication Adherence: Taking medications as prescribed and monitoring their effectiveness.
Conclusion
Type 2 diabetes is a manageable condition with the right approach to lifestyle, medication, and monitoring. By understanding the symptoms, causes, and treatment options, individuals with Type 2 diabetes can lead healthy, active lives. Continuous education and support, along with advancements in medical technology, offer hope and improved quality of life for those affected by this condition.
For more information and support, consult healthcare providers or join diabetes support groups. Stay informed and proactive in managing Type 2 diabetes to ensure optimal health and well-being.



