Diabetes is a chronic health condition that affects millions of people worldwide. Despite its prevalence, there remains a significant amount of misinformation and misunderstanding about the disease. This blog aims to provide a clear and comprehensive guide to understanding diabetes, its types, symptoms, management, and the importance of lifestyle choices in its prevention and control.
1. What is Diabetes?
Diabetes is a chronic condition characterized by elevated levels of blood glucose (or blood sugar), which occurs when the body either does not produce enough insulin or cannot effectively use the insulin it produces. Insulin is a hormone produced by the pancreas that allows cells to take in glucose from the bloodstream and use it for energy. Without proper insulin function, glucose accumulates in the blood, leading to various health problems over time.
If you want to adopt 4 components strategy, Call us @ 9773935777 or visit:- Diabetes Care Home
2. How Does Insulin Work?
To understand diabetes, it’s crucial to understand the role of insulin:
- Glucose Absorption: When we eat, our bodies break down carbohydrates into glucose, which enters the bloodstream.
- Insulin Release: In response to rising glucose levels, the pancreas releases insulin.
- Glucose Uptake: Insulin acts as a key, allowing glucose to enter cells, particularly muscle and liver cells, to be used for energy or stored for future use.

Pre-Diabetes
Pre-diabetes is a condition where blood glucose levels are higher than normal but not high enough to be classified as type 2 diabetes. It’s a critical stage where lifestyle changes can prevent the progression to type 2 diabetes.
Long-term Effects of Uncontrolled Diabetes
Without proper management, diabetes can lead to severe complications:
- Cardiovascular Disease: Increases the risk of heart disease, stroke, and hypertension.
- Nerve Damage (Neuropathy): Can cause pain, tingling, and loss of sensation, especially in the feet.
- Kidney Damage (Nephropathy): Can lead to kidney failure or end-stage kidney disease.
- Eye Damage (Retinopathy): Can cause blindness.
- Foot Damage: Poor circulation and nerve damage can lead to foot sores and infections, sometimes requiring amputation.
- Skin Conditions: Diabetes can make you more susceptible to skin

3. Types of Diabetes
Type 1 diabetes is an autoimmune condition that results in the body’s inability to produce insulin, a hormone crucial for regulating blood glucose levels. Unlike other forms of diabetes, type 1 is not related to lifestyle factors such as diet or exercise but is instead caused by the immune system attacking the insulin-producing beta cells in the pancreas.

Causes and Risk Factors of Type 1 Diabetes
The exact cause of type 1 diabetes is still unknown, but several factors are believed to contribute to its development:
- Genetic Predisposition: Certain genes increase the risk of developing type 1 diabetes.
- Autoimmune Reaction: The immune system mistakenly identifies the beta cells as harmful and destroys them.
- Environmental Factors: Possible triggers such as viral infections or other environmental factors may play a role in the onset of type 1 diabetes.
Symptoms of Type 1 Diabetes
Type 1 diabetes often develops rapidly and symptoms can appear suddenly. Common symptoms include:
- Increased Thirst and Frequent Urination: Excess glucose in the bloodstream pulls fluid from tissues, leading to dehydration and frequent urination.
- Extreme Hunger: Despite eating more, the body’s inability to utilize glucose properly leads to persistent hunger.
- Unintended Weight Loss: The body starts breaking down fat and muscle for energy, resulting in weight loss.
- Fatigue and Weakness: Lack of glucose in cells makes it difficult for the body to function properly, causing tiredness.
- Blurred Vision: High blood sugar levels can cause the lens of the eye to swell, leading to vision problems.
- Slow-Healing Sores and Frequent Infections: High blood glucose can impair the body’s ability to heal and fight infections.

Diagnosis of Type 1 Diabetes
Diagnosis of type 1 diabetes involves several tests:
- Glycated Hemoglobin (A1C) Test: Measures the average blood glucose level over the past 2-3 months. An A1C level of 6.5% or higher indicates diabetes.
- Random Blood Sugar Test: A blood sample taken at a random time. A level of 200 milligrams per deciliter (mg/dL) or higher suggests diabetes.
- Fasting Blood Sugar Test: Measures blood glucose after an overnight fast. A fasting blood sugar level of 126 mg/dL or higher indicates diabetes.
- Autoantibody Tests: Detect specific autoantibodies that are often present in type 1 diabetes but not in type 2.
If you want to adopt 4 components strategy, Call us @ 9773935777 or visit:- Diabetes Care Home
Management and Treatment of Type 1 Diabetes
Management of type 1 diabetes involves a comprehensive approach to maintain blood glucose levels within the target range. This includes:
- Insulin Therapy: Since the body cannot produce insulin, regular insulin injections or an insulin pump are necessary. Types of insulin include rapid-acting, short-acting, intermediate-acting, and long-acting.
- Continuous Glucose Monitoring (CGM): Devices that track blood sugar levels throughout the day and night, providing real-time data and alerts for high and low blood glucose levels.
- Blood Sugar Monitoring: Regular self-monitoring using a glucose meter to check blood sugar levels.
- Healthy Diet: A balanced diet that includes a mix of carbohydrates, proteins, and fats. Carbohydrate counting helps manage blood glucose levels.
- Regular Physical Activity: Exercise helps lower blood glucose levels and improve insulin sensitivity.
- Education and Support: Ongoing education about diabetes management and access to support from healthcare providers, dietitians, and diabetes educators.

Living with Type 1 Diabetes
Living with type 1 diabetes requires continuous monitoring and management, but with the right strategies, individuals can lead full, active lives. Key aspects include:
- Routine and Structure: Establishing a daily routine for meals, insulin administration, and physical activity.
- Stress Management: Stress can affect blood glucose levels, so techniques such as mindfulness, relaxation exercises, and adequate sleep are important.
- Community and Support: Joining support groups and connecting with others who have type 1 diabetes can provide emotional support and practical tips.

Advances and Research of Type 1 Diabetes
Ongoing research in type 1 diabetes aims to improve treatment options and work towards a cure. Some promising areas include:
- Artificial Pancreas: Systems that automate insulin delivery based on continuous glucose monitoring.
- Beta Cell Transplantation: Research into transplanting healthy beta cells into individuals with type 1 diabetes.
- Immunotherapy: Investigating ways to prevent or halt the autoimmune process that destroys beta cells.
Type 1 diabetes is a challenging condition, but with proper management, individuals can maintain good health and a high quality of life. Advances in technology and treatment options continue to improve the outlook for those living with type 1 diabetes. Education, support, and proactive management are essential components in navigating life with this condition.
2. Understanding Type 2 Diabetes
Type 2 diabetes is a chronic condition that affects the way the body processes blood glucose, or sugar. Unlike type 1 diabetes, which is characterized by the body’s inability to produce insulin, type 2 diabetes is primarily a result of the body’s resistance to insulin or insufficient insulin production.

Causes and Risk Factors of Type 2 diabetes
Type 2 diabetes develops due to a combination of genetic and lifestyle factors:
- Insulin Resistance: The body’s cells become resistant to the effects of insulin, meaning more insulin is required to achieve the same effect. Over time, the pancreas cannot keep up with the increased demand.
- Genetics: Family history of diabetes significantly increases the risk.
- Obesity: Excess weight, particularly around the abdomen, is a major risk factor. Fat cells can trigger inflammation and insulin resistance.
- Inactivity: A sedentary lifestyle contributes to insulin resistance and obesity.
- Unhealthy Diet: Diets high in processed foods, sugar, and unhealthy fats can increase the risk.
- Age: Risk increases with age, particularly after 45, although it is increasingly seen in younger populations.
- Ethnicity: Certain ethnic groups, including African Americans, Hispanics, Native Americans, and Asian Americans, have a higher risk.
Symptoms of Type 2 diabetes
Type 2 diabetes often develops slowly, and symptoms may be mild or absent in the early stages. Common symptoms include:

- Increased Thirst and Frequent Urination: Excess sugar in the bloodstream causes fluid to be pulled from tissues, leading to dehydration and frequent urination.
- Increased Hunger: The body’s inability to utilize glucose properly can lead to increased hunger.
- Weight Loss: Despite eating more, the body may lose weight as it uses fat and muscle for energy.
- Fatigue: Lack of glucose in cells can cause tiredness and weakness.
- Blurred Vision: High blood sugar levels can affect the eyes.
- Slow-Healing Sores: Poor circulation and high blood glucose levels can impair healing.
- Frequent Infections: High blood sugar levels can weaken the immune system.
If you want to adopt 4 components strategy, Call us @ 9773935777 or visit:- Diabetes Care Home
How To Diagnose Type 2 diabetes
Diagnosis of type 2 diabetes involves several tests:
- Glycated Hemoglobin (A1C) Test: Measures the average blood glucose level over the past 2-3 months. An A1C level of 6.5% or higher indicates diabetes.
- Fasting Blood Sugar Test: Measures blood glucose after an overnight fast. A level of 126 mg/dL or higher suggests diabetes.
- Oral Glucose Tolerance Test: Measures blood sugar before and two hours after consuming a sugary drink. A level of 200 mg/dL or higher after two hours indicates diabetes.
- Random Blood Sugar Test: A random blood sugar level of 200 mg/dL or higher suggests diabetes.
Management and Treatment
Management of type 2 diabetes involves lifestyle changes, monitoring, and medication:

- Healthy Eating: A balanced diet rich in whole grains, fruits, vegetables, lean proteins, and healthy fats is crucial. Carbohydrate counting and understanding the glycemic index of foods can help manage blood sugar levels.
- Regular Physical Activity: Exercise improves insulin sensitivity and helps lower blood sugar levels. Aim for at least 150 minutes of moderate-intensity exercise per week.
- Weight Management: Achieving and maintaining a healthy weight can improve blood glucose control and reduce the need for medications.
- Monitoring Blood Sugar Levels: Regular monitoring helps manage blood glucose levels and adjust treatment plans as needed.
- Medications: Depending on the severity, various medications can be prescribed, including:
- Metformin: Helps reduce glucose production in the liver and improve insulin sensitivity.
- Sulfonylureas: Stimulate the pancreas to produce more insulin.
- DPP-4 Inhibitors: Help reduce blood sugar levels without causing hypoglycemia.
- GLP-1 Receptor Agonists: Slow digestion and increase insulin production.
- SGLT2 Inhibitors: Help the kidneys remove glucose from the bloodstream.
- Insulin Therapy: In some cases, insulin therapy may be necessary.
Complications of Type 2 Diabetes
Uncontrolled type 2 diabetes can lead to serious complications:
- Cardiovascular Disease: Increased risk of heart disease, stroke, and hypertension.
- Nerve Damage (Neuropathy): Can cause pain, tingling, and loss of sensation, especially in the extremities.
- Kidney Damage (Nephropathy): Can lead to kidney failure or end-stage kidney disease.
- Eye Damage (Retinopathy): Can lead to blindness if untreated.
- Foot Damage: Poor circulation and nerve damage can lead to serious foot infections and even amputation.
- Skin Conditions: Increased risk of bacterial and fungal infections.
- Hearing Impairment: Higher blood sugar levels can damage nerves in the ears.
Preventing Type 2 Diabetes
While type 2 diabetes is largely preventable, lifestyle modifications can significantly reduce the risk:

- Maintain a Healthy Weight: Aim for a healthy body weight to improve insulin sensitivity.
- Eat a Balanced Diet: Focus on whole foods, fiber-rich vegetables, lean proteins, and healthy fats.
- Stay Active: Regular physical activity helps maintain a healthy weight and improve insulin sensitivity.
- Avoid Smoking: Smoking increases the risk and its complications.
- Limit Alcohol Consumption: Excessive alcohol intake can lead to weight gain and increase blood sugar levels.
Type 2 diabetes is a manageable condition with the right approach to diet, exercise, and medication. Understanding the disease, recognizing its symptoms, and making necessary lifestyle changes are crucial steps in managing and preventing type 2 diabetes. With proactive management, individuals with type 2 diabetes can lead healthy and fulfilling lives. Advances in research and treatment continue to improve the outlook for those living with this condition.
What are the differences between type 1 and type 2 diabetes?

| Feature | Type 1 | Type 2 |
| Nature of Disease | Autoimmune condition | Metabolic disorder involving insulin resistance |
| Insulin Production | Little to no insulin production | Insulin resistance followed by decreased insulin production |
| Age of Onset | Typically childhood or adolescence | Typically adulthood, increasingly seen in children |
| Risk Factors | Genetic predisposition, environmental factors, possible viral infections | Genetic predisposition, obesity, physical inactivity, poor diet |
| Symptoms Onset | Sudden and severe | Gradual and often subtle |
| Common Symptoms | Increased thirst, frequent urination, extreme hunger, weight loss, fatigue, blurred vision | Similar to Type 1 but often less pronounced: increased thirst, frequent urination, hunger, weight gain, fatigue, blurred vision |
| Management | Insulin therapy, blood sugar monitoring, diet, exercise | Lifestyle changes (diet and exercise), oral medications, insulin therapy (if necessary), blood sugar monitoring |
| Body Weight | Usually normal or underweight | Often overweight or obese |
| Ketoacidosis Risk | High | Low, but can occur in severe cases |
| Prevalence | About 5-10% of all cases | About 90-95% of all cases |
| Prevention | Not currently preventable | Can often be prevented or delayed with lifestyle changes |
| Long-term Risks | Cardiovascular disease, neuropathy, nephropathy, retinopathy | Cardiovascular disease, neuropathy, nephropathy, retinopathy, often exacerbated by obesity and metabolic syndrome |
| Family History | Family history may increase risk | Strong familial link, especially with a family history of type 2 diabetes |
3. Gestational Diabetes
Gestational diabetes is a type of diabetes that develops during pregnancy. It typically occurs in the second or third trimester and usually resolves after the baby is born. However, it can have significant health implications for both the mother and the baby if not managed properly.

Causes and Risk Factors of Gestational Diabetes
The exact cause of gestational diabetes is not known, but several factors contribute to its development:
- Hormonal Changes: During pregnancy, the placenta produces hormones that can interfere with the body’s ability to use insulin effectively, leading to insulin resistance.
- Increased Insulin Demand: As the pregnancy progresses, the body’s insulin needs increase. If the pancreas cannot produce enough insulin to meet these needs, blood glucose levels rise.
If you want to adopt 4 components strategy, Call us @ 9773935777 or visit:- Diabetes Care Home
Risk factors for gestational diabetes include:
- Age: Women over 25 are at a higher risk.
- Weight: Being overweight or obese increases the risk.
- Family History: A family history of diabetes increases the risk.
- Previous Gestational Diabetes: Having gestational diabetes in a previous pregnancy.
- Ethnicity: Higher prevalence in African American, Hispanic, Native American, and Asian American women.
- Polycystic Ovary Syndrome (PCOS): Women with PCOS are at higher risk.
Symptoms of Gestational Diabetes
Gestational diabetes often does not cause noticeable symptoms. However, some women may experience:

- Increased Thirst and Frequent Urination: Similar to other types of diabetes, excess glucose in the blood can cause dehydration and frequent urination.
- Fatigue: High blood sugar levels can lead to feeling tired and weak.
- Blurred Vision: Elevated blood glucose can affect vision.
Diagnosis of Gestational Diabetes
It is a typically diagnosed through screening tests during pregnancy:
- Glucose Challenge Test (GCT): A preliminary screening test where the pregnant woman drinks a glucose solution, and blood sugar levels are measured after one hour. If blood sugar levels are higher than normal, further testing is required.
- Oral Glucose Tolerance Test (OGTT): If the GCT results are abnormal, an OGTT is conducted. The woman fasts overnight, then her blood sugar is measured before and after drinking a glucose solution at one, two, and three-hour intervals. A diagnosis of gestational diabetes is made if two or more of the readings are above the normal range.
Also Read:- The 5 Essential Components of Diabetes Management Strategy
Management and Treatment
Managing gestational diabetes involves monitoring and controlling blood sugar levels to ensure a healthy pregnancy and delivery:
- Healthy Diet: Eating a balanced diet rich in whole grains, fruits, vegetables, and lean proteins. Carbohydrate counting and choosing low-glycemic index foods can help control blood sugar levels.
- Regular Physical Activity: Exercise helps lower blood sugar levels and improve insulin sensitivity. Activities such as walking, swimming, and prenatal yoga are often recommended.
- Monitoring Blood Sugar Levels: Regularly checking blood sugar levels helps manage gestational diabetes and make necessary adjustments to diet or treatment.
- Medications: If diet and exercise are not enough to control blood sugar levels, insulin therapy or oral medications may be prescribed.
- Frequent Medical Check-ups: Regular monitoring by healthcare providers to track the health of both mother and baby.
Complications of Gestational Diabetes
If not properly managed, gestational diabetes can lead to complications for both the mother and the baby:

For the Baby:
- Macrosomia: High birth weight due to excess glucose crossing the placenta, increasing the risk of delivery complications.
- Premature Birth: Higher risk of early labor.
- Respiratory Distress Syndrome: Difficulty breathing at birth due to immature lungs.
- Hypoglycemia: Low blood sugar levels after birth.
- Increased Risk of Obesity and Type 2 Diabetes: Babies born to mothers with gestational diabetes have a higher risk of developing obesity and type 2 diabetes later in life.
For the Mother:
- High Blood Pressure and Preeclampsia: Increased risk of pregnancy-related high blood pressure.
- Cesarean Delivery: Higher likelihood of needing a C-section due to delivery complications.
- Future Diabetes: Increased risk of developing type 2 diabetes later in life.
How To Prevent Gestational Diabetes
While it is not always possible to prevent gestational diabetes, certain lifestyle changes can reduce the risk:
- Maintain a Healthy Weight: Achieving a healthy weight before pregnancy and gaining weight within recommended limits during pregnancy.
- Healthy Diet: Eating a balanced diet that is low in sugar and refined carbohydrates and high in fiber.
- Regular Exercise: Engaging in regular physical activity before and during pregnancy.
- Regular Medical Check-ups: Early and regular prenatal care to monitor health and manage any potential issues.

Gestational diabetes is a common pregnancy complication that requires careful management to ensure the health of both the mother and the baby. By understanding the risk factors, symptoms, and management strategies, expectant mothers can take proactive steps to control their blood sugar levels and reduce the risk of complications. With proper care and lifestyle adjustments, most women with gestational diabetes can have healthy pregnancies and deliveries.
If you want to adopt 4 components strategy, Call us @ 9773935777 or visit:- Diabetes Care Home
Symptoms of Diabetes
Diabetes is a condition characterized by high blood sugar levels, which, if left untreated, can lead to various complications. Recognizing the symptoms of diabetes early is crucial for effective management and prevention of further health issues. The symptoms can vary depending on the type of diabetes and the individual, but there are common signs to be aware of.

Common Symptoms
- Increased Thirst (Polydipsia): High blood sugar levels cause the body to pull fluid from tissues, leading to dehydration. This results in an increased need to drink water.
- Frequent Urination (Polyuria): The kidneys work overtime to filter and absorb the excess glucose. When they can’t keep up, the excess glucose is excreted into the urine, pulling fluids from the tissues and causing frequent urination.
- Extreme Hunger (Polyphagia): Despite eating, people with diabetes often feel intense hunger because their bodies cannot use the glucose from their food properly.
- Unexplained Weight Loss: Even though individuals may eat more, they may lose weight. This is because the body starts breaking down muscle and fat for energy due to the inability to use glucose efficiently.
- Fatigue: The lack of glucose in cells means they cannot function optimally, leading to feelings of tiredness and fatigue.
- Blurred Vision: High blood sugar levels can cause the lens of the eye to swell, leading to blurred vision.
- Slow-Healing Sores or Frequent Infections: Diabetes can impair blood flow and the body’s ability to heal, making infections more frequent and slower to resolve.
Tingling or Numbness in Hands or Feet (Neuropathy):High blood sugar can cause nerve damage, leading to tingling, pain, or numbness in the extremities.
When to See a Doctor
It’s important to see a healthcare provider if you experience any of the following:
- Frequent urination and excessive thirst.
- Unexplained weight loss.
- Extreme hunger and fatigue.
- Blurred vision.
- Slow-healing sores or frequent infections.
- Tingling or numbness in hands or feet.

Early detection and management of diabetes can prevent serious complications and improve quality of life. Regular check-ups and screening are essential, especially for those with risk factors for diabetes.
Recognizing the symptoms of diabetes is the first step towards effective management and prevention of complications. If you or someone you know is experiencing these symptoms, it is crucial to seek medical advice promptly. Early diagnosis and intervention can make a significant difference in the management of diabetes and the overall health of individuals.
Risk Factors
Diabetes is influenced by a variety of genetic, lifestyle, and environmental factors. Understanding these risk factors can help in early identification and prevention of the disease. Here, we will discuss the risk factors associated with the three main types of diabetes: type 1, type 2, and gestational diabetes.
Risk Factors for Type 1
Type 1 diabetes is primarily an autoimmune condition where the body’s immune system attacks and destroys insulin-producing beta cells in the pancreas. The exact cause is unknown, but several factors increase the risk:

- Family History: Having a parent or sibling with type 1 diabetes increases the risk.
- Genetics: Certain genes are associated with a higher risk of type 1 diabetes.
- Geography: Incidence of type 1 diabetes tends to be higher in countries farther from the equator.
- Age: Although type 1 diabetes can appear at any age, it commonly manifests in children, adolescents, and young adults.
- Viral Infections: Exposure to certain viruses, such as the Coxsackievirus, Epstein-Barr virus, or cytomegalovirus, may trigger the autoimmune response.
- Early Dietary Factors: Some studies suggest that early exposure to cow’s milk or cereal proteins might be linked to an increased risk, though evidence is not conclusive.
Risk Factors for Type 2
Type 2 diabetes is primarily related to insulin resistance and relative insulin deficiency. Several factors contribute to its development:

- Weight: Being overweight or obese is a significant risk factor, particularly if the weight is carried around the abdomen.
- Inactivity: Lack of physical activity contributes to weight gain and insulin resistance.
- Family History: Having a parent or sibling with type 2 diabetes increases the risk.
- Age: The risk increases with age, especially after 45, though type 2 diabetes is increasingly seen in younger populations.
- Ethnicity: Higher risk is observed in certain ethnic groups, including African Americans, Hispanics, Native Americans, Asian Americans, and Pacific Islanders.
- Gestational Diabetes History: Women who had gestational diabetes during pregnancy have a higher risk of developing type 2 diabetes later.
- Polycystic Ovary Syndrome (PCOS): Women with PCOS have an increased risk due to associated insulin resistance.
- High Blood Pressure: Hypertension is often associated with type 2 diabetes.
- Abnormal Cholesterol Levels: Low levels of HDL (“good”) cholesterol and high levels of triglycerides increase the risk.
- Pre-diabetes: Blood glucose levels that are higher than normal but not yet high enough to be diagnosed as diabetes.
- Unhealthy Diet: Diets high in sugar, refined carbohydrates, and unhealthy fats contribute to weight gain and insulin resistance.
If you want to adopt 4 components strategy, Call us @ 9773935777 or visit:- Diabetes Care Home
Risk Factors for Gestational Diabetes
Gestational diabetes occurs during pregnancy and typically resolves after childbirth. The following factors increase the risk:

- Age: Women over 25 are at a higher risk.
- Weight: Being overweight or obese increases the likelihood.
- Family History: A family history of diabetes increases the risk of gestational diabetes.
- Ethnicity: Higher prevalence in African American, Hispanic, Native American, and Asian American women.
- Previous Gestational Diabetes: Having gestational diabetes in a previous pregnancy increases the risk in subsequent pregnancies.
- Polycystic Ovary Syndrome (PCOS): Women with PCOS are at higher risk.
- Excessive Weight Gain During Pregnancy: Gaining more weight than recommended during pregnancy can increase the risk.
- High Blood Pressure: Preexisting hypertension can elevate the risk.
- Unhealthy Diet: Diets high in sugar and refined carbohydrates can contribute to the development of gestational diabetes.
Additional Risk Factors
There are also general factors that can increase the risk of developing any type of diabetes:
- Stress: Chronic stress can affect blood sugar levels and insulin sensitivity.
- Smoking: Smoking increases the risk of diabetes and its complications.
- Sleep Disorders: Poor sleep quality and sleep apnea are associated with insulin resistance and type 2 diabetes.
- Sedentary Lifestyle: Lack of physical activity contributes to obesity and insulin resistance.
Understanding the risk factors for diabetes can help in early detection and preventive measures. While some risk factors like genetics and age are beyond our control, many lifestyle-related factors can be managed through healthy diet, regular exercise, and maintaining a healthy weight. For those with higher risk due to family history or other non-modifiable factors, regular monitoring and proactive healthcare can help in early identification and management of diabetes. By addressing these risk factors, individuals can significantly reduce their chances of developing diabetes and its associated complications.
Proactive Steps for Reducing Risk
To mitigate the risk of developing diabetes, consider the following steps:

- Maintain a Healthy Weight: Aim for a balanced diet and regular exercise to keep your weight in a healthy range.
- Stay Active: Engage in at least 150 minutes of moderate-intensity exercise per week, such as walking, cycling, or swimming.
- Eat a Balanced Diet: Focus on whole grains, fruits, vegetables, lean proteins, and healthy fats. Limit intake of refined sugars and carbohydrates.
- Monitor Your Health: Regular check-ups with your healthcare provider can help detect early signs of diabetes. If you have risk factors, ask about screening tests.
- Avoid Smoking: If you smoke, seek help to quit. Smoking increases the risk of diabetes and other chronic diseases.
- Limit Alcohol Consumption: Excessive drinking can contribute to weight gain and affect blood sugar levels.
- Manage Stress: Practice stress-reducing techniques such as meditation, yoga, or deep-breathing exercises.
- Get Adequate Sleep: Aim for 7-9 hours of quality sleep per night to maintain overall health and well-being.
Recognizing and understanding the risk factors for diabetes is crucial for prevention and early intervention. By making informed lifestyle choices and staying vigilant about your health, you can significantly reduce your risk of developing diabetes and lead a healthier, more fulfilling life. If you have concerns about your risk factors, speak with a healthcare provider who can guide you through personalized prevention strategies and monitoring plans.
If you want to adopt 4 components strategy, Call us @ 9773935777 or visit:- Diabetes Care Home
How To Manage Diabetes
Effective diabetes management is essential to maintain blood glucose levels within the target range and prevent complications. Management strategies involve lifestyle modifications, regular monitoring, and medication. Here’s a comprehensive guide to managing diabetes:
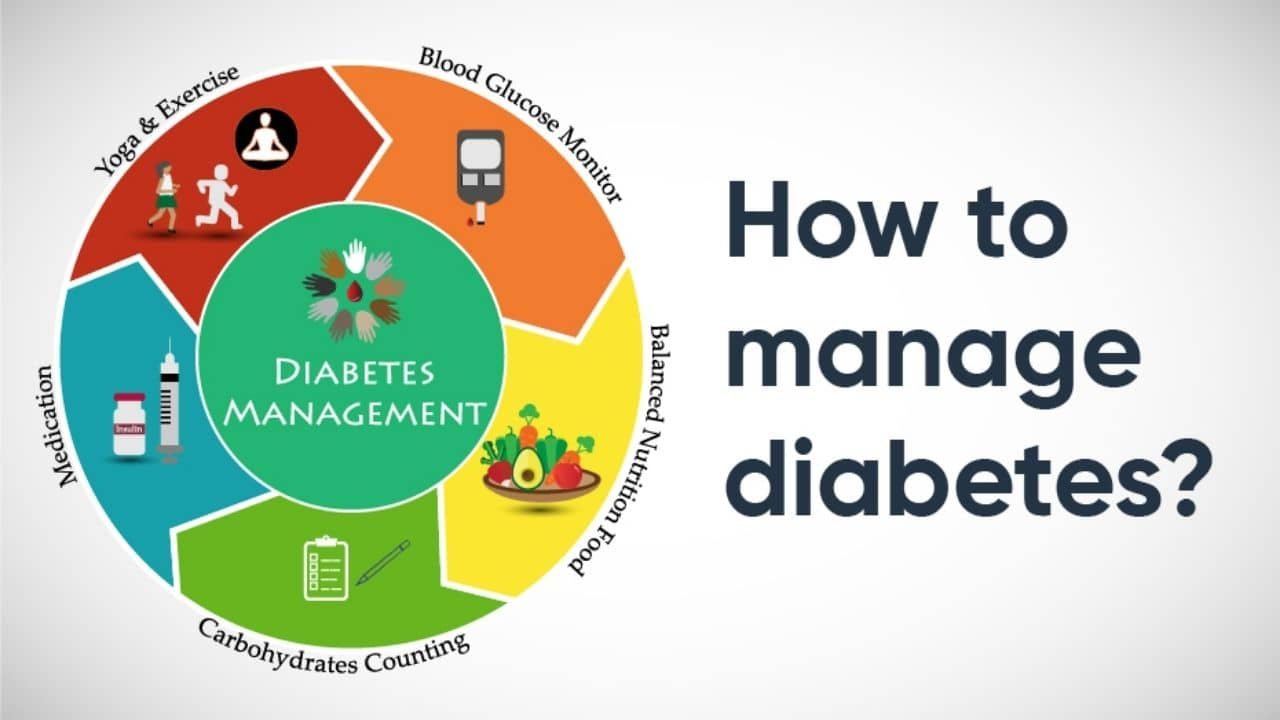
Lifestyle Modifications
1. Healthy Eating
- Balanced Diet: Focus on whole grains, fruits, vegetables, lean proteins, and healthy fats. Avoid processed foods and sugars.
- Carbohydrate Counting: Monitor carbohydrate intake to manage blood sugar levels. Work with a dietitian to understand how different foods affect your blood sugar.
- Portion Control: Eating smaller, more frequent meals can help maintain steady blood sugar levels.
- Glycemic Index: Choose foods with a low glycemic index (GI), which have a slower, more gradual effect on blood sugar levels.
2. Regular Physical Activity
- Exercise: Aim for at least 150 minutes of moderate-intensity aerobic exercise per week, such as walking, swimming, or cycling. Include strength training exercises twice a week.
- Consistency: Regular physical activity helps improve insulin sensitivity and maintain a healthy weight.
- Monitoring: Check blood sugar levels before and after exercise to understand how your body responds to physical activity.
3. Weight Management
- Healthy Weight: Achieving and maintaining a healthy weight can improve blood sugar control and reduce the risk of complications.
- Diet and Exercise: Combine a balanced diet with regular exercise to reach and maintain your weight goals.
4. Stress Management
- Stress Reduction: Practice stress management techniques such as mindfulness, meditation, yoga, and deep-breathing exercises. Chronic stress can affect blood sugar levels.
- Sleep: Ensure adequate sleep (7-9 hours per night) to maintain overall health and well-being.
Monitoring Blood Sugar Levels
- Self-Monitoring: Use a blood glucose meter to regularly check your blood sugar levels. Your healthcare provider will advise how often you need to test.
- Continuous Glucose Monitoring (CGM): A CGM device can provide real-time blood sugar readings and trends throughout the day and night.
- Recording Results: Keep a log of your blood sugar levels, medication doses, food intake, and physical activity. This helps you and your healthcare provider make informed decisions about your treatment plan.
Medication
1. Insulin Therapy (Primarily for Type 1 and Some Type 2 Diabetes)
- Types of Insulin: Includes rapid-acting, short-acting, intermediate-acting, and long-acting insulin. Your healthcare provider will determine the right type and dosage for you.
- Delivery Methods: Insulin can be administered through injections or an insulin pump.
2. Oral Medications (Primarily for Type 2 Diabetes)
- Metformin: Reduces glucose production in the liver and improves insulin sensitivity.
- Sulfonylureas: Stimulate the pancreas to produce more insulin.
- DPP-4 Inhibitors: Help reduce blood sugar levels without causing hypoglycemia.
- SGLT2 Inhibitors: Help the kidneys remove glucose from the bloodstream.
- GLP-1 Receptor Agonists: Slow digestion and increase insulin production.
Regular Healthcare Check-ups

- Medical Appointments: Regular visits to your healthcare provider to monitor your diabetes management plan and make necessary adjustments.
- Blood Tests: Regular A1C tests to measure your average blood sugar levels over the past 2-3 months. The target A1C level for most adults is below 7%.
- Eye Exams: Regular eye exams to check for diabetic retinopathy and other eye issues.
- Foot Exams: Regular foot exams to check for sores, infections, or other complications.
- Blood Pressure and Cholesterol Checks: Monitoring and managing blood pressure and cholesterol levels to reduce the risk of cardiovascular complications.
If you want to adopt 4 components strategy, Call us @ 9773935777 or visit:- Diabetes Care Home
Education and Support
- Diabetes Education: Attend diabetes education programs to learn about managing your condition effectively.
- Support Groups: Joining a support group can provide emotional support and practical tips from others who have diabetes.
Emergency Preparedness
- Hypoglycemia: Recognize the signs of low blood sugar (such as shaking, sweating, confusion) and know how to treat it quickly with fast-acting carbohydrates.
- Sick Day Plan: Have a plan in place for managing your diabetes when you are ill, as illness can affect blood sugar levels.
Managing diabetes involves a comprehensive approach that includes lifestyle modifications, regular monitoring, medication, and ongoing education. By staying proactive and working closely with your healthcare team, you can effectively manage your diabetes and maintain a high quality of life. Regular follow-ups and a supportive network are essential components of successful diabetes management.
Complications of Diabetes
if not well managed, can lead to a variety of serious complications affecting multiple organs and systems in the body. These complications can be acute or chronic, and they significantly impact the quality of life and overall health of individuals with diabetes.
Acute Complications
1. Hypoglycemia
Definition: Abnormally low blood sugar levels, typically below 70 mg/dL.
Symptoms: Shakiness, sweating, confusion, irritability, dizziness, hunger, headache, and in severe cases, loss of consciousness or seizures.
Management: Immediate consumption of fast-acting carbohydrates like glucose tablets, juice, or candy. Monitoring blood sugar levels regularly and adjusting medications or insulin accordingly.
2. Diabetic Ketoacidosis (DKA)
Definition: A serious condition where the body starts breaking down fats at an abnormal rate, producing ketones, leading to acidic blood.
Symptoms: High blood sugar levels, ketones in the urine, frequent urination, extreme thirst, nausea, vomiting, abdominal pain, fruity-scented breath, and confusion.
Management: Requires urgent medical treatment with fluids, electrolytes, and insulin. Regular monitoring of blood sugar and ketone levels to prevent DKA.
3. Hyperosmolar Hyperglycemic State (HHS)
Definition: A dangerous condition characterized by extremely high blood sugar levels without the presence of ketones.
Symptoms: Very high blood sugar levels (often above 600 mg/dL), excessive thirst, dry mouth, frequent urination, warm, dry skin, fever, drowsiness, and confusion.
Management: Immediate medical attention with intravenous fluids and insulin. Monitoring blood sugar levels to prevent HHS.
Chronic Complications
1. Cardiovascular Disease
Risk: Increased risk of heart disease, heart attack, stroke, and high blood pressure.
Management: Controlling blood sugar, blood pressure, and cholesterol levels. Adopting a heart-healthy diet, exercising regularly, and avoiding smoking.
2. Nerve Damage (Neuropathy)
Types: Peripheral neuropathy (affects feet and hands), autonomic neuropathy (affects internal organs), and focal neuropathy (affects specific nerves).
Symptoms: Numbness, tingling, pain, weakness, digestive issues, sexual dysfunction, and urinary problems.
Management: Blood sugar control, pain management, medications, and physical therapy.
3. Kidney Damage (Nephropathy)
Risk: Diabetes can damage the blood vessels in the kidneys, leading to chronic kidney disease or kidney failure.
Symptoms: Often no symptoms until significant damage occurs, but can include swelling in the feet and ankles, high blood pressure, and changes in urination.
Management: Regular screening for kidney function, blood sugar and blood pressure control, medications, and potentially dialysis or kidney transplant in severe cases.
4. Eye Damage (Retinopathy)
Risk: Damage to the blood vessels in the retina, which can lead to blindness.
Symptoms: Blurred vision, floaters, dark areas of vision, and vision loss.
Management: Regular eye exams, blood sugar control, managing blood pressure and cholesterol, laser treatment, and injections.
5. Foot Damage
Risk: Poor circulation and nerve damage increase the risk of foot ulcers and infections, which can lead to amputation.
Symptoms: Ulcers, sores, blisters, infections, and numbness in the feet.
Management: Regular foot care, inspecting feet daily, wearing comfortable shoes, and seeking prompt medical attention for any foot issues.
6. Skin Conditions
Risk: Diabetes can make the skin more susceptible to bacterial and fungal infections.
Symptoms: Bacterial infections (boils, styes), fungal infections (athlete’s foot, ringworm), and itchy skin.
Management: Good skin hygiene, moisturizing regularly, monitoring for skin changes, and treating infections promptly.
7. Hearing Impairment
Risk: Diabetes can damage the nerves and blood vessels in the ears, leading to hearing loss.
Symptoms: Difficulty hearing, needing to increase the volume on electronic devices, and frequently asking others to repeat themselves.
Management: Regular hearing tests and using hearing aids if necessary.
8. Alzheimer’s Disease
Risk: Type 2 may increase the risk of dementia and Alzheimer’s disease.
Management: Blood sugar control, heart-healthy lifestyle, mental exercises, and regular medical check-ups.
Preventing Complications
Preventing complications involves meticulous management of diabetes:
- Regular Monitoring: Frequent blood sugar checks and A1C tests to keep levels within target ranges.
- Healthy Lifestyle: Balanced diet, regular physical activity, maintaining a healthy weight, and avoiding tobacco.
- Medications: Adhering to prescribed medications for diabetes, blood pressure, and cholesterol.
- Regular Medical Visits: Routine check-ups with healthcare providers, eye exams, foot exams, and kidney function tests.
- Education: Staying informed about diabetes management and recognizing early signs of complications.
The complications can significantly impact quality of life and lead to severe health issues if not managed properly. Through vigilant monitoring, a healthy lifestyle, and regular medical care, many of these complications can be prevented or managed effectively, allowing individuals with diabetes to lead healthy and active lives.
If you want to adopt 4 components strategy, Call us @ 9773935777 or visit:- Diabetes Care Home
Understanding Diabetes Mellitus
Diabetes Mellitus is a chronic metabolic disorder characterized by elevated blood glucose levels, resulting from either insufficient insulin production by the pancreas or the body’s inability to effectively use the insulin it produces. This condition can lead to serious health complications if not properly managed. Diabetes Mellitus is classified primarily into three types: Type 1, Type 2, and Gestational Diabetes.

Types of Diabetes Mellitus
1. Type 1 Diabetes Mellitus
Type 1 is an autoimmune condition where the body’s immune system attacks and destroys the insulin-producing beta cells in the pancreas. As a result, the body produces little to no insulin. It typically manifests in childhood or adolescence but can occur at any age.
Causes: The exact cause is unknown but involves genetic predisposition and environmental factors, such as viral infections.
Symptoms: Increased thirst, frequent urination, hunger, weight loss, fatigue, and blurred vision.
Management: Requires lifelong insulin therapy, blood sugar monitoring, dietary management, and regular exercise.
2. Type 2 Diabetes Mellitus
Type 2 diabetes is the most common form of diabetes, accounting for about 90-95% of all cases. It is primarily characterized by insulin resistance, where the body’s cells do not respond effectively to insulin, and later, an inadequate insulin production.
Causes: A combination of genetic factors, obesity, physical inactivity, and poor dietary habits.
Symptoms: Similar to Type 1 diabetes but often less pronounced and can develop slowly, including increased thirst, frequent urination, hunger, weight gain, fatigue, and blurred vision.
Management: Lifestyle changes (diet and exercise), oral medications, and sometimes insulin therapy. Regular monitoring of blood sugar levels is crucial.
3. Gestational Diabetes Mellitus
Gestational diabetes occurs during pregnancy and usually resolves after childbirth. It increases the risk of developing Type 2 diabetes later in life for both the mother and the child.
Causes: Hormonal changes during pregnancy that affect insulin function, along with genetic and lifestyle factors.
Symptoms: Often asymptomatic but can include increased thirst, frequent urination, fatigue, and nausea.
Management: Diet and exercise, blood sugar monitoring, and sometimes insulin therapy or oral medications. Regular prenatal care is essential.
Symptoms of Diabetes Mellitus
Regardless of the type, common symptoms of diabetes include:
- Increased Thirst (Polydipsia): Excess glucose in the bloodstream causes dehydration, leading to increased thirst.
- Frequent Urination (Polyuria): The kidneys work to expel excess glucose through urine, leading to frequent urination.
- Extreme Hunger (Polyphagia): Despite eating, the body’s cells are not receiving glucose, leading to persistent hunger.
- Unexplained Weight Loss: The body starts using fat and muscle for energy due to lack of insulin.
- Fatigue: Lack of glucose in the cells results in low energy levels.
- Blurred Vision: High blood sugar levels can cause fluid to be pulled from the lenses of the eyes.
- Slow-Healing Sores or Frequent Infections: High glucose levels can impair blood circulation and the immune system.
Complications of Diabetes Mellitus
If not properly managed, diabetes can lead to serious complications, including:
- Cardiovascular Disease: Increased risk of heart disease, stroke, and high blood pressure.
- Neuropathy: Nerve damage leading to pain, tingling, and numbness, particularly in the extremities.
- Nephropathy: Kidney damage that can lead to kidney failure.
- Retinopathy: Eye damage that can result in blindness.
- Foot Damage: Poor circulation and nerve damage increase the risk of foot ulcers and infections.
- Skin Conditions: Higher susceptibility to bacterial and fungal infections.
- Hearing Impairment: Higher risk of hearing problems.
- Alzheimer’s Disease: Increased risk of cognitive decline and dementia.
Management of Diabetes Mellitus
Effective management of diabetes involves a combination of lifestyle changes, regular monitoring, and medication:
- Healthy Diet: Emphasize whole grains, fruits, vegetables, lean proteins, and healthy fats. Avoid processed foods and sugars.
- Regular Exercise: Aim for at least 150 minutes of moderate-intensity exercise per week.
- Weight Management: Achieve and maintain a healthy weight.
- Blood Sugar Monitoring: Regularly check blood glucose levels to keep them within target ranges.
- Medications: Use of insulin or oral medications as prescribed by a healthcare provider.
- Regular Medical Check-ups: Routine visits to monitor overall health and manage any complications.
Diabetes Mellitus is a complex and chronic condition requiring diligent management to prevent complications and maintain a good quality of life. Through lifestyle modifications, medication, and regular monitoring, individuals can effectively manage their condition and lead healthy lives. Early diagnosis and proactive management are key to reducing the risk of serious health issues associated with diabetes.
Conclusion
Diabetes is a complex and multifaceted disease that requires diligent management and lifestyle adjustments. With the right approach, individuals with diabetes can lead healthy and fulfilling lives. Education and awareness are critical in managing and preventing this condition, making it essential for everyone to understand the basics of diabetes and the importance of a healthy lifestyle.
For those living with this problem, it’s vital to stay informed and proactive in your care. And for those at risk, taking preventive measures can significantly impact your health and well-being.
FAQs About Diabetes
1. What are the different types of diabetes?
Answer: The main types are:
– Type 1 Diabetes: An autoimmune condition where the body’s immune system attacks insulin-producing cells in the pancreas.
– Type 2 Diabetes: A condition characterized by insulin resistance and eventual insulin deficiency.
– Gestational Diabetes: Diabetes that develops during pregnancy and usually resolves after childbirth.
2. What are the common symptoms of diabetes?
Answer: Common symptoms include:
– Increased thirst and frequent urination
– Extreme hunger
– Unexplained weight loss
– Fatigue
– Blurred vision
– Slow-healing sores or frequent infections
3. How is diabetes diagnosed?
Answer: This can be diagnosed through blood tests, including:
– Fasting Blood Sugar Test: Measures blood glucose after an overnight fast.
– A1C Test: Provides an average blood sugar level over the past 2-3 months.
– Oral Glucose Tolerance Test: Measures blood sugar before and after drinking a glucose-rich beverage.
4. What causes Type 1 diabetes?
Answer: Type 1 diabetes is caused by an autoimmune reaction where the body’s immune system mistakenly attacks the insulin-producing beta cells in the pancreas. The exact trigger is unknown but may involve genetic and environmental factors, such as viral infections.
5. Can Type 2 diabetes be prevented?
Answer: Yes, Type 2 diabetes can often be prevented or delayed through lifestyle changes, such as maintaining a healthy weight, engaging in regular physical activity, eating a balanced diet, and avoiding smoking.
6. What is gestational diabetes and how is it managed?
Answer: Gestational diabetes occurs during pregnancy and is usually managed through diet and exercise, blood sugar monitoring, and sometimes insulin or oral medications. It typically resolves after childbirth, but women who have had gestational diabetes are at higher risk of developing Type 2 later in life.
7. What treatments are available for Type 1 diabetes?
Answer: Treatment for Type 1 includes:
– Insulin Therapy: Administered through injections or an insulin pump.
– Blood Sugar Monitoring: Regular checking of blood glucose levels.
– Diet and Exercise: Maintaining a healthy diet and regular physical activity.
8. What are the potential complications of unmanaged diabetes?
Answer: It can lead to serious complications, including:
– Cardiovascular disease
– Nerve damage (neuropathy)
– Kidney damage (nephropathy)
– Eye damage (retinopathy)
– Foot problems, such as ulcers and infections
– Skin conditions and infections
– Hearing impairment
9. How can I manage my blood sugar levels effectively?
Answer: Effective blood sugar management involves:
– Healthy Eating: Following a balanced diet rich in whole grains, fruits, vegetables, lean proteins, and healthy fats.
– Regular Exercise: Engaging in at least 150 minutes of moderate-intensity exercise per week.
– Medication Adherence: Taking prescribed medications or insulin as directed.
– Regular Monitoring: Checking blood glucose levels regularly and keeping track of results.
10. What precautions should I take?
Answer: Precautions for managing diabetes include:
– Regular Medical Check-ups: Routine visits to your healthcare provider to monitor and manage your condition.
– Foot Care: Inspecting your feet daily for any signs of sores or infections and wearing comfortable shoes.
– Eye Exams: Regular eye exams to detect and treat any early signs of retinopathy.
– Vaccinations: Staying up-to-date with vaccinations, as diabetes can increase the risk of infections.
– Stress Management: Practicing stress reduction techniques such as mindfulness, yoga, or meditation to help maintain stable blood sugar levels.



